Key Facts
- Endometriosis occurs when tissue similar to the lining of the uterus is found outside the normal location.
- Symptoms are usually bad period cramps and pelvic pain.
- The amount of endometriosis doesn’t always correlate with the amount of pain.

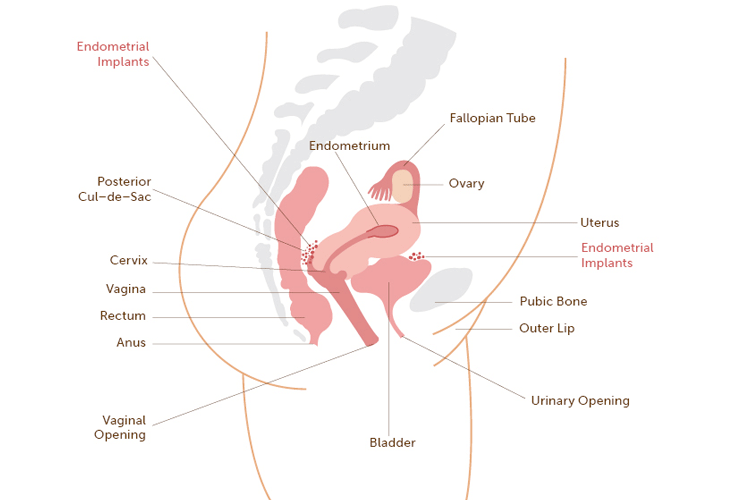
Endometriosis is an inflammatory condition that occurs when tissue similar to the lining of the uterus is found outside its normal location. Common locations of endometrial implants include the ovaries, fallopian tubes, ligaments that support the uterus, and tissue covering the bladder and rectum. The location of the endometrial implants and the way in which the lesions affect the pelvic organs contribute to the symptoms that both adolescent and adults have.
What are the symptoms of endometriosis?
Endometriosis causes different symptoms. Some people may have one or more of the following symptoms:
- Severe period cramps
- Chronic pelvic pain that comes and goes (throughout the menstrual cycle)
- Painful urination (pain when peeing)
- Diarrhea or constipation (loose or less bowel movements)
- Pelvic pain with exercise
- Pain after a pelvic exam
- Pain with intercourse (if sexually active)
The amount of endometriosis doesn’t always compare to the amount of pain a person may have. For example: Some people may have a lot of endometriosis and have very little pain, while others who have a small amount of endometriosis have severe pain.
How is endometriosis diagnosed?
The ONLY way to diagnosis endometriosis for sure is to have a procedure called a laparoscopy. This procedure allows a doctor to look inside the pelvic cavity with a special lens to check for endometriosis (implants). Other tests that are often ordered before a laparoscopy may include blood tests, vaginal cultures (to check for infection), an ultrasound and/or an MRI. These tests are done to “rule out” other possible causes of pelvic pain.
What causes endometriosis?
Although we know that some young women are more likely to develop endometriosis because one or more of their female relatives have it, we still do not know what causes the disease.
The three most accepted theories are:
- Sampson’s Theory: This theory explains that the flow of menstrual blood gets “backed up” causing some of the blood to flow in a reverse direction. This process causes blood containing endometrial tissue to attach to surfaces outside of the uterus.
- Meyer’s Theory: This theory proposes that specific cells (that are present at birth) called “metaplastic cells” change into endometrial cells.
- Vascular Theory: This theory suggests that the endometrial tissue “travels” through the body via the blood vessels. It then implants in the abdomen and grows, resulting in pain.
How is endometriosis treated?
If someone has severe menstrual cramps and/or pelvic pain that causes them to miss school, their doctor may want them to have a diagnostic laparoscopy. If endometriosis is found, treatment falls into the following categories:
- Observation: Keeping track of symptoms and trying mild pain medicine is usually recommended first.
- Lifestyle changes: Exercise, a healthy diet, and getting enough rest helps to manage pain. Relaxation techniques such as yoga and meditation can also help.
- Medical suppression: Hormonal treatment works by shutting off hormones made by the ovaries, which temporarily stops a person’s menstrual cycle and lowers the estrogen level.
- Surgery: A special instrument is inserted into a tiny incision or cut in the abdomen (near thenavel) while the person is asleep under anesthesia. Visible endometriosis is destroyed or removed.
- Pain treatment services: Your friend, (sibling or partner) may be referred for pain treatment services where they may be evaluated for physical therapy, biofeedback, or another technique to help with pain control.
- Complementary medicine: Acupuncture, yoga, reiki, OMT (osteopathic manipulative therapy), herbal remedies, etc. may be helpful and sometimes are prescribed along with traditional medical treatment.
The goals of treatment should be aimed at relieving pain, controlling the progression of endometriosis and preserving fertility for future childbearing. Comprehensive and early treatment can make a big difference in improving a young person’s quality of life.
How can I be helpful?
It’s important to have a clear understanding of endometriosis; the symptoms, treatment, the possible side effects of each medicine, and how the disease impacts your friend’s (sibling, or partner’s) life. Letting them know that you want to help and being supportive will make a huge difference in the way she copes with her disease. You can be supportive by learning about their disease, being a good listener, and showing them that you care.
Here are some examples of how you can show support:
- Keep in touch: Text, e-mail, or call; especially on the days your friend (sibling, or partner) is absent from school.
- Take notes: Offer to pick up or drop off school work and copy notes in classes you share.
- Bring the social event to your friend’s house: If you’re planning a get together with mutual friends and your friend isn’t up to going out (because of pain), consider meeting at them home.
- Learn signs:Figure out a way that your friend can communicate when they are in pain. Having someone who understands their pain threshold will likely give them confidence to socialize.
What else do I need to know about endometriosis?
- Youngpeople CAN suffer from symptoms of endometriosis.
- Endometriosis is NOT an STI (sexually transmitted infection).
- Chronic pelvic pain is NOT normal. Most young people have none or mild menstrual cramps one or two days a month. If your friend (sibling, or partner) is absent from school or work a lot because of pelvic pain and/or menstrual cramps or has pain in their lower abdomen (belly) that isn’t relieved with over-the-counter pain medicine, tell her to make an appointment with their health care provider.
- Endometriosis occurs among young and older people of ALL RACES
- Getting pregnant does NOT cure this disease, but may improve symptoms for some people. Some people with endometriosis who have given birth continue to have pain.
Frequently Asked Questions:
What is it like to live with endometriosis?
Having endometriosis can definitely add to the everyday stress of being a teen or young adult.
- People with endometriosis have a significant amount of pelvic pain and menstrual cramps.
- A young person’s pain is often misunderstood, perhaps because they dont necessarily “look sick”.
- People with endo often miss school and frequently turn down social invitations because of pain. This can lead to feelings of isolation and depression.
How common is endometriosis among teens born with female reproductive organs?
It’s not uncommon for a young person to have endometriosis. If endometriosis runs in the family, a young person may be more likely to have it than someone else with no family history. A research study done at Boston Children’s Hospital found that endometriosis was the most common diagnosis for people with chronic pelvic pain who had undergone a diagnostic laparoscopy.
How often does a young person need to be seen by her GYN (gynecology) team?
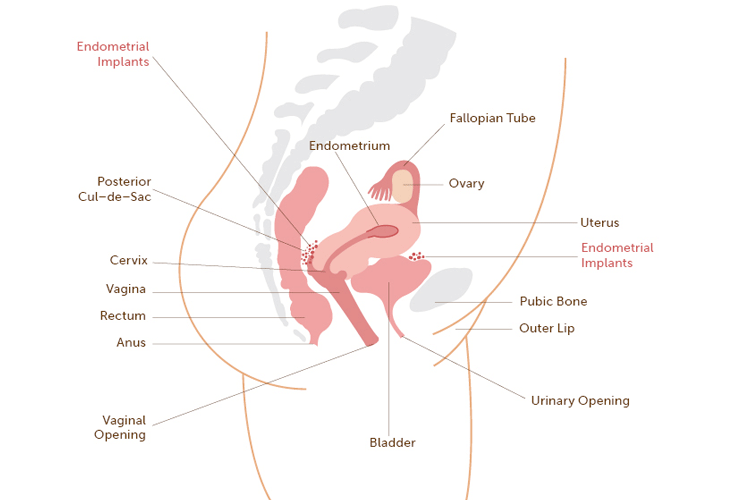
This depends on: the type of medication they are prescribed, how well they responds to treatment, and whether or not she has other gynecological issues. For example, if they are on a medicine called Lupron Depot®, they will need to return for their shots either monthly, or every three months, depending on the prescribed dose. If they are being treated with birth control pills, they will likely have follow-up appointments about every three months. They may return earlier than their scheduled appointments if they experiences side effects or feels the pain is not getting better. At the very least, they will need to have a check-up with their gynecologist once a year.
If a young person is on birth control pills for endometriosis, does it mean she’s having sex?
Birth control pills (also called hormone pills, oral contraceptives or “the Pill”) are almost always prescribed to young people with endometriosis. Being on the pill does not mean that the person is having sex.
How can I help my friend get to school?
One of the primary goals of treatment is to successfully manage your friend’s (sibling, or partner’s) pain. Their treatment plan is specially designed to lessen their symptoms that often get in the way of going to school, participating in activities, and socializing with friends. You can encourage your friend (sibling, or partner) to go to school even if it means going in later or getting dismissed early. If they are absent, you could offer to pick up school-work for them.
You can help your friend or loved one by understanding THEIR experience with endometriosis and having trusting and ongoing conversations about what she is going through.
How can I help my friend (sibling, or partner) get out and do things?
Understanding what your friend (sibling, or partner) is experiencing in terms of pain will help you know why they may feel anxious about going out. You can let them know that you will be with them and that she has the option of going home early if they are in pain.
Sometimes plans you have made with your friend, sibling, or partner may need to be adjusted because they are tired or in pain. This doesn’t necessarily mean that you can’t get together. Choosing more relaxing activities, or meeting at their house is better than not including them in your plans.
How can I tell if my friend (sibling, or partner) is depressed?
If your friend, sibling, partners or someone you love is having trouble sleeping, is not interested in social activities, has a loss of appetite and/or change in weight, they may be depressed. It’s important to tell your friend’s (or partner’s) parents/guardians and encourage them to make an appointment with their GYN team. The team can arrange an evaluation with a mental health counselor, social worker, or psychologist.
Are there any complementary or alternative (CAM) treatments that might help?
Although there is limited data that supports the effectiveness of CAM therapy in the treatment of endometriosis, some research studies suggest that CAM therapies such as acupuncture, pelvic floor physical therapy, transcutaneous electrical nerve stimulator (TENS) unit, and yoga are helpful in controlling pelvic pain. Pain Treatment Centers are often located in major hospitals and provide services to evaluate young people with endometriosis. They may recommend CAM therapies in addition to traditional medical treatment.
Watching your friend, sibling, or partner deal with pain (from endometriosis) and the possible side effects of treatment can be very hard especially if you feel you can’t do anything to make them feel better. Remember, your role as a friend, sibling or partner is very important, as you can be of great support and inspiration.


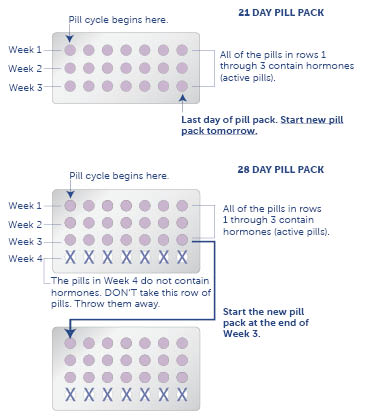
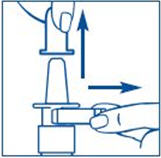
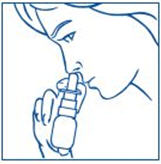
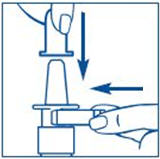
 Nafarelin acetate is the generic name for “Synarel,” a medicine that is used to treat endometriosis. It is a type of gonatropin-releasing hormone agonist (GnRH agonist) medicine. GnRH agonist medicines help to lessen pelvic pain caused by endometriosis.
Nafarelin acetate is the generic name for “Synarel,” a medicine that is used to treat endometriosis. It is a type of gonatropin-releasing hormone agonist (GnRH agonist) medicine. GnRH agonist medicines help to lessen pelvic pain caused by endometriosis.






 Young people with endometriosis usually have certain symptoms. The following quiz was created to help you find out if you have one or more of the most common symptoms associated with endometriosis. This quiz is designed as an educational tool and is not a substitute for medical advice by your health care providers. The only way to diagnose endometriosis is to have a surgical procedure called a laparoscopy.
Young people with endometriosis usually have certain symptoms. The following quiz was created to help you find out if you have one or more of the most common symptoms associated with endometriosis. This quiz is designed as an educational tool and is not a substitute for medical advice by your health care providers. The only way to diagnose endometriosis is to have a surgical procedure called a laparoscopy.