Key Facts
- Bacterial Vaginosis (BV) is the most common cause of vaginal discharge.
- People who are born with a female reproductive system, who are sexually active are more likely to get BV than people who are not sexually active.
- Medication can cure BV, but remember to take ALL of it – even if the symptoms go away.
- Do NOT drink alcohol while taking oral Metronidazole pills (one of the treatments for BV).
- Using condoms lessens the chance of getting a BV infection.
People born with a female reproductive system, at any age can have Bacterial vaginosis or “BV” – rarely in teens and people who have never been sexually active. However, it is much more common among young people and adults and who have had sex with one or more partners.
What causes bacterial vaginosis?
Bacterial vaginosis or “BV” is a vaginal infection caused by an overgrowth of anaerobic bacteria and an organism called Gardnerella vaginalis. “Anaerobic” means the bacteria doesn’t need any oxygen to survive or grow. Small amounts of these anaerobic bacteria and Gardnerella can normally be found in your vagina. Bacterial vaginosis occurs when the balance of organisms in your vagina is upset and the anaerobic bacteria overgrow. The good, protective bacteria Lactobacilli are then outnumbered and not able to do their normal job, which is to make a natural disinfectant which helps keep organisms at the normal, healthy balance in your vagina. When this happens, an infection occurs.
The exact reasons that bacteria overgrow are not known. BV is more common in women who have multiple sexual partners. BV may also occur after sexual intercourse with a new partner and after douching and changing the bacteria in the vagina.
What are the signs/symptoms of bacterial vaginosis (BV)?
It’s a fact that 50-75% of people who have BV don’t have any symptoms, but those who do often complain of a fishy smelling vaginal odor and a thin, grayish-white vaginal discharge. The discharge may be light or heavy. The odor may get worse around the time of menstruation or after unprotected sexual intercourse. When semen (sperm) mixes with vaginal secretions, the odor becomes stronger. Less common symptoms include: vaginal itchiness, redness, and pain with intercourse.
Your health care provider may notice vaginal discharge or odor during your routine pelvic exam and do a test of the vaginal fluid to see if you have BV or any other vaginal infections. If you do have BV, your health care provider will give you a prescription to treat it.
How is bacterial vaginosis (BV) diagnosed?
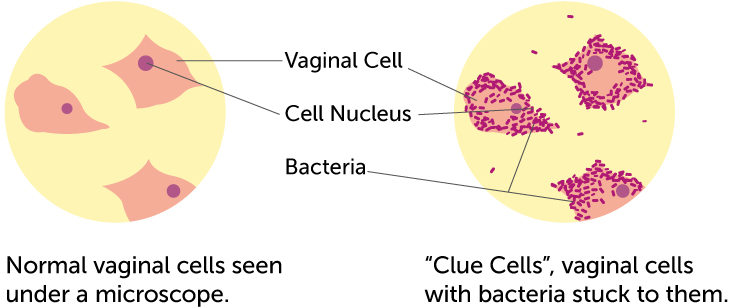
The only way to diagnose BV is with an exam by your health care provider (HCP) and testing the vaginal discharge. Your HCP will use a cotton swab to take a sample of your vaginal discharge. The acidity of the discharge is then measured with pH paper. If your vagina is less acidic than it should be (pH of more than 4.5), this may be a sign that you may have bacterial vaginosis. Your HCP can look at the sample under a microscope. If the normal bacteria (lactobacilli) are not there but many “clue” cells (cells from the vaginal lining that are coated with bacteria) are present, then you likely have bacterial vaginosis. Your health care provider will check to see if you have at least 3 out of 4 of the following symptoms:
- Thin white discharge
- Clue cells
- pH>4.5
- Fishy odor (from discharge)
There are also special office tests that can help make the diagnosis.
How is bacterial vaginosis (BV) treated?
If you have bacterial vaginosis, your health care provider will likely either give you a prescription for a cream or gel that you put into your vagina with an applicator or a prescription for pills that you take by mouth. You should let your HCP know about any other medications that you are taking. If you use a vaginal cream or gel, you should NOT use tampons during the treatment because it will absorb the medication and make it less effective. Metronidazole or clindamycin are the two most common prescription medicines prescribed to treat bacterial vaginosis. Both medications are effective, but you need to make sure that you take ALL of the medicine for it to work. Secnidazole is a single- dose pill that is used to treat BV. It typically costs more but it is not more effective (than metronidazole or clindamycin). Many people choose the vaginal gel because the pills can cause nausea and a metal taste in your mouth. Others prefer the oral medication because they don’t want to insert a cream in the vagina. Both help treat BV.
- You should NOT douche or use vaginal deodorant sprays. Although they may help cover up the odor, they will not cure the infection, and they can make your infection worse.
- Condoms may help to lessen the chance of getting BV if you are sexually activebecause the semen doesn’t change the bacteria in the vagina. Even though BV is more common in teens and adolescents who have sexual intercourse with many partners, treatment of a partner who was born with a male reproductive system does not prevent future BV infections.
Can I get bacterial vaginosis again?
Unfortunately, bacterial vaginosis often comes back, even if you take all of your medication and follow the advice of your health care provider (HCP). According to research studies, 30% of people who got better after treatment had BV again within three months, and more than 50% of people had BV again within 12 months. Experts don’t know exactly why this happens. If your symptoms come back, see your HCP. You may need to be treated for a longer period of time.
Can bacterial vaginosis cause any other problems?
Bacterial vaginosis can increase your chance of getting a serious pelvic infection called pelvic inflammatory disease (PID), or an infection after a vaginal or uterus operation. It may also increase your chance of having premature delivery (delivery before the normal 9 months).
Are there any complications from bacterial vaginosis if it’s not treated?
Most of the time BV is treated and doesn’t cause any problems. However, there are some risks you should know about. You may also be more likely to get other sexually transmitted infections.
BV can increase the risk of pelvic inflammatory disease, which can cause fertility problems later. Pregnant women who have BV are more likely to have premature babies. Whether treatment of BV during pregnancy prevents premature births is still unclear. The Center for Disease Control (CDC) recommends treatment of BV if you are having symptoms or if you are having vaginal or uterus surgery.
Our health guides are developed through a systematic, rigorous process to ensure accuracy, reliability, and trustworthiness. Written and reviewed by experienced healthcare clinicians from Boston Children's Hospital, a Harvard Medical School teaching hospital and consistently ranked as a top hospital by Newsweek and U.S. News & World Report, these guides combine clinical expertise, specialized knowledge, and evidence-based medicine. We also incorporate research and best practices from authoritative sources such as the CDC, NIH, PubMed, top medical journals, and UpToDate.com. Clinical specialists and subject matter experts review and edit each guide, reinforcing our commitment to high-quality, factual, scientifically accurate health information for young people.

