Why is there no cure for endometriosis?
Although medical researchers have been working for years to identify a cure for endometriosis, as of right now, there is no cure. This is because the exact cause remains unknown. The good news is that researchers around the world are investigating factors that might explain why one woman gets endo and another woman does not, such as: whether exposure to certain environmental agents cause endo, and if the immune system reacts a certain way to make a woman more at risk. Researchers have also been working on identifying a “gene” that would help recognize women more likely to be diagnosed with endo. Some doctors claim that they can “cure” endometriosis with surgery. This is NOT true as they cannot see the microscopic disease that is present and therefore they cannot remove all of the disease. Until a cure for endometriosis is discovered, there are effective treatments to control pain caused from endo, and preserve fertility.
How do I deal with the fact that there is no cure for my daughter’s endo?
It’s normal to feel frustrated, angry, sad, or other emotions when you know that nothing can be done at this time to cure your daughter’s endo. You may find it reassuring to know that there are treatments to control her symptoms and prevent her endo from getting worse. Research is always moving ahead and the possibility of a cure could very well be in the near future.
How common is endometriosis among teen girls?
We know that it is not uncommon for young women to have endometriosis. If endometriosis runs in the family, a young woman may be more likely to have it than someone else with no family history. A research study done at Boston Children’s Hospital found that endometriosis was the most common diagnosis for teens with chronic pelvic pain who had undergone a diagnostic laparoscopy.
How often will the gynecologist see my daughter?
Many factors influence how often your daughter will be followed by her GYN team: the type of medication she is prescribed, how well she responds to treatment, and whether or not she has other gynecological issues. If your daughter is being treated for her pain with birth control pills, she will probably need to return about 3 months after she starts her pills. Typically, if your daughter is on Lupron Depot®, she will need to return for her shot either once a month or every three months depending on the prescribed dose. She may return earlier if she is experiencing side effects or she feels that her endo symptoms are not improving. When she is doing well and is happy with her medical treatment, she will need to have an annual appointment for a GYN check–up and to obtain a prescription refill.
How do I help my daughter comply with her treatment plan?
Your daughter’s compliance with her treatment plan relies on a good balance between assuming responsibility for her treatment, and your support. Support may include your assistance with the practical parts of her treatment plan, such as filling prescriptions, communicating with schools and transportation to appointments. Asking adolescents to assume increasing amounts of responsibility can be stressful, but it is a necessary part of growing up. Honest communication with your daughter about taking increased responsibility for her health care encourages her to be compliant with her medical treatment.
If my daughter goes on birth control pills for her endometriosis, am I giving her permission to have sex?
No. If your daughter is offered birth control pills for the treatment of her endometriosis, it is because birth control pills are effective in reducing pelvic pain. The treatment will not change your daughter’s values about sexually activity. This is a good opportunity, however, to talk to your daughter about your concerns and expectations.
How can I help my daughter live with endometriosis without it interfering with school and social activities?
One of the primary goals of your daughter’s treatment is to successfully manage her pain. The goal of her treatment plan should be to reduce the symptoms that interfere with her education, activities, and social life.
How can I help my daughter maintain consistent school attendance?
Some young women with endometriosis experience an unusually high number of school absences due to chronic pelvic pain. Pain management is key when treating endometriosis so that your daughter can attend school and participate in social activities. If her pain is particularly bad in the morning, you may choose to give her the option of going to school late rather than being absent for the entire day. In rare cases when school absences are high, it may be necessary to work with the school system to arrange for a home tutor. It is important to communicate about extended school absences with your daughter’s gynecologist.
When should I let my daughter stay home from school (because of endo pain)?
There may be times when, despite the best of treatment plans and efforts, your daughter feels that the pain from her endometriosis is intolerable and requires her to stay home. It would be most helpful if the criteria for staying out of school or other activities were established BEFORE the situation arises. For example, if your expectations are clear about her school attendance, class work, and homework, it will be easier for her to take responsibility when she is absent from school due to her endometriosis. If you feel your daughter is falling behind in her classes and/or homework due to frequent absences, or that her pain interferes with completing assignments, make an appointment with her school counselor or advisor before she falls too far behind. Health care providers may be able to help by advocating for necessary support services so that your daughter can have a successful school year.
If your daughter is experiencing sleep difficulties, disinterest in social activities, decreased appetite and/or change in weight, she may be depressed. It is important to make an appointment with her health care provider to discuss options for an evaluation with a mental health counselor, social worker, or psychologist.
Are there any alternative or complementary treatments that will help my daughter?
Complementary and alternative medicine or “CAM” therapies have become popular in the last decade. Although there is limited data that supports the effectiveness of herbs, acupuncture, and other forms of CAM therapy in the treatment of endometriosis, new research studies are underway to determine if in fact these therapies are helpful. Pain Treatment Centers in major hospitals will evaluate young women with endometriosis and often recommend CAM therapies in addition to traditional medical treatment. If you choose to explore options on your own, make sure that the CAM provider is a licensed professional and inform all of your daughter’s health care providers what herbs or therapies the CAM practitioner prescribes.
How will the endometriosis affect my daughter’s sexuality?
Every gynecological condition by definition focuses on the reproductive system and this necessitates conversations about sexuality. This often makes young women and their parents uncomfortable. Young women with endometriosis may have more intense feelings about their sexuality because of all the medical attention they receive to this part of their body. As a parent, you can use this opportunity to have honest discussions with your daughter about sex and the choices she will make.
How will the endometriosis affect my daughter’s fertility in the future?
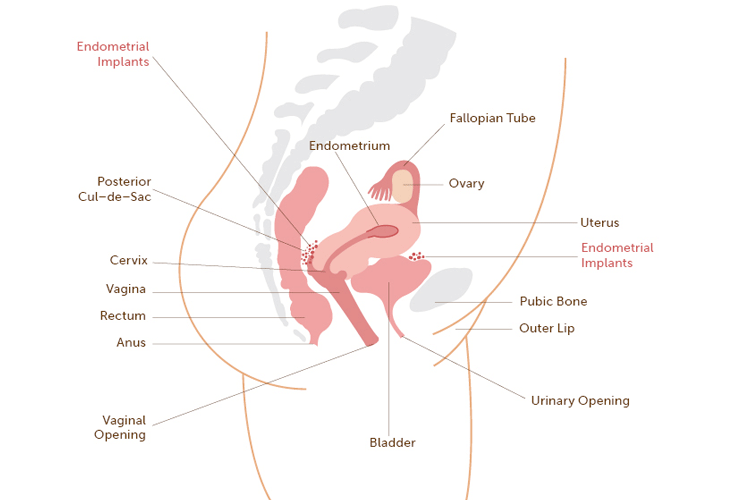
Early treatment is important in the relief of pain but also in the prevention of the natural progression of endometriosis that in some cases may cause infertility. Infertility commonly results when endometriosis causes changes in the pelvic organs and/or the fallopian tubes. Since endometriosis is a chronic (life–long) disease, it’s important for your daughter to have early treatment to preserve her fertility. Your daughter should be followed for her endometriosis throughout her childbearing years.
Why does my daughter need to have surgery and medicine for her endo?
Endometriosis can only be diagnosed by laparoscopy. At the time of a laparoscopy, great care is taken to destroy any visible endo lesions (also called implants) and any adhesions. Some endometriosis isn’t visible, yet it responds well to medication. That’s why her doctor combines medical and surgical therapy to treat this disease.
A study done by Dr. Marc Laufer and colleagues at Boston Children’s Hospital and published in the Journal of Pediatric and Adolescent Gynecology (2009) 22:257–263 concluded that there is supporting evidence that standard combined surgical–medical management in adolescents does in fact retard disease progression.
Will my daughter ever need another laparoscopy?
The need for another laparoscopy depends on many factors, such as when her last procedure was, if she’s having a problem with pain control while taking medication, and if her gynecologist feels it’s necessary to check to see if her endometriosis has grown. If she does require another laparoscopy in the future, the endometriosis lesions will be removed and/or destroyed. The goal is always to lower her pain and preserve her fertility,
In an earlier study at Boston Children’s Hospital. Dr. Laufer and his colleagues were interested to find out if they would see more endometriosis at the time of a second laparoscopy (in young women with diagnosed endometriosis). They found that endometriosis did not get worse (didn’t grow) in patients who were treated with both surgery and medication.
Will my daughter need to have her uterus and/or ovaries removed because she has endometriosis?
No. She will NOT need to have her uterus and/or ovaries removed (hysterectomy). All treatment will be aimed at relieving pain and preserving her ability to have children someday.
Will my daughter be able to get pregnant?
Not being able to get pregnant (infertility) can result if endometriosis causes changes to your daughter’s pelvic organs, including her fallopian tubes and ovaries. With early treatment, endometriosis should not interfere with her ability to become pregnant (when she is ready).
Should my daughter get pregnant to cure her endo?
No. There is no cure for endometriosis at this time. Some women who are pregnant may experience less endo–related symptoms during their pregnancy while others may have no change or a worsening of symptoms. For women who have an improvement with their symptoms (while they are pregnant), the effects are usually temporary.
How long does my daughter need to be followed for her endo?
Endometriosis is a chronic condition that requires long–term medical treatment and follow–up, especially during her childbearing years. Many factors affect how often she will need to be seen by her gynecologist, such as whether or not she is responding to treatment. Since there is no cure for endometriosis at this time, she will need to be on medication. Therefore, follow–up visits with her gynecologist will need to be made periodically. Refills for prescription medications (for endometriosis) are provided at this time.
If I have another daughter, should she get checked for endometriosis?
Women are more likely to develop endometriosis if a close female relative from their mom or dad’s side has it. Likewise, if one daughter has been diagnosed with endometriosis, and your other daughter(s) has painful periods and pelvic pain at other times during her menstrual cycle that interferes with school and social activities, it is a good idea that she has a gynecological evaluation.
 The best thing you can do to understand your daughter’s diagnosis is to learn all you can about endometriosis. It’s helpful for both you and your daughter to maintain an ongoing list of questions for your daughter’s GYN team. The doctors, nurses, and social workers will assist you and your daughter in understanding her diagnosis and the treatment options at all stages of her treatment.
The best thing you can do to understand your daughter’s diagnosis is to learn all you can about endometriosis. It’s helpful for both you and your daughter to maintain an ongoing list of questions for your daughter’s GYN team. The doctors, nurses, and social workers will assist you and your daughter in understanding her diagnosis and the treatment options at all stages of her treatment.